Aquagenic Urticaria: Comprehensive Clinical Review INGA314.com analysis
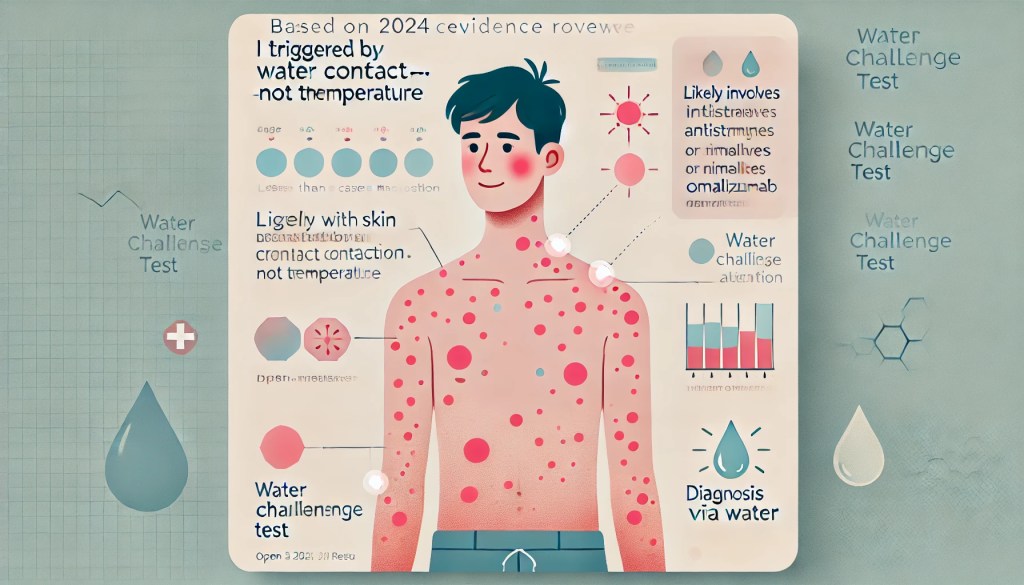
Aquagenic urticaria (AU) is an extremely rare physical urticaria characterized by pruritic wheals after skin contact with water, irrespective of temperature or source. Documented cases number fewer than 100 globally; however, underdiagnosis is likely due to limited awareness and misclassification. This review synthesizes current knowledge from peer-reviewed literature (2019–2024), offering practical diagnostic criteria, evidence-informed treatment algorithms with acknowledged variability, and patient management guidelines.
Epidemiology
- Prevalence: <100 documented cases; likely underdiagnosed
- Gender: Female-to-male ratio approximately 3:1
- Onset: Typically around puberty; documented cases from early childhood (4 years old) to adulthood
- Familial Link: ~18% familial occurrence, indicating potential genetic factors
Clinical Presentation
Symptoms
- Small wheals (1–3 mm) with surrounding erythema
- Onset within 10–30 minutes after water exposure
- Resolution within 30–60 minutes post-drying (though exceptions exist)
- Common sites: neck, shoulders, arms, trunk
- Rare systemic involvement (e.g., wheezing, anaphylaxis)
Diagnostic Criteria
- Characteristic wheals post-water contact
- Positive water challenge test (wet compress or limb immersion at ~35°C selected for standardization purposes)
- Exclusion of other physical urticarias
Differential Diagnoses
- Cholinergic urticaria
- Aquagenic pruritus
- Cold/Heat urticaria
- Pressure urticaria
- Dermographism
- Systemic mastocytosis
Illustrative Case Studies
- 19-year-old male: Good response to fexofenadine (180 mg)
- 4-year-old male: Positive response to ketotifen syrup
- Teenage female: Refractory symptoms resolved with omalizumab (300 mg monthly)
- 28-year-old female: Severe systemic involvement with anaphylaxis and lupus (SLE), requiring immunosuppressants
Pathophysiological Hypotheses
- Water-soluble epidermal antigen activation
- Sebum-water interaction hypothesis
- Osmotic pressure changes triggering mast cells
- Epidermal barrier dysfunction
- Acetylcholine-mediated mast cell activation
- IgE-mediated reaction (supported strongly by omalizumab efficacy; however, inconsistent responses indicate multiple mechanisms may coexist)
Treatment Strategies
First-Line Treatments
- Second-generation H₁ antihistamines (cetirizine, fexofenadine, loratadine)
- Dose escalation (up to 4× standard dose, considering potential side effects)
Second-Line Treatments
- H₁ and H₂ antihistamine combination
- Mast cell stabilizers (ketotifen, cromolyn sodium)
- Barrier creams (petroleum-based)
- Leukotriene receptor antagonists (montelukast)
Third-Line Treatments
- Omalizumab (300 mg monthly)
- Phototherapy (narrowband UVB)
- Anticholinergics (scopolamine)
- Immunosuppressants (for autoimmune-associated cases)
Treatment Algorithm (Subject to clinical judgment and individual patient response)
- Confirm diagnosis via water challenge
- Initiate second-generation H₁ antihistamine
- Escalate dosage cautiously if response insufficient
- Consider second-line therapies based on response
- Employ omalizumab or phototherapy for refractory cases
Prognosis and Quality of Life
- Prognosis varies widely, with some spontaneous improvements documented
- Significant psychological and lifestyle impacts, including anxiety, avoidance behaviors, and social isolation
- Psychological support and practical adaptations crucial for management
Research Directions
Clinical Research
- Global AU registry establishment
- Longitudinal outcomes and standardized reporting
Basic Science Research
- Skin biopsy analysis during active lesions
- Genetic studies of familial AU
- IgE profiling in responders to omalizumab
Therapeutic Research
- Structured N-of-1 trials
- Combination therapy protocols
Practical Guidelines for Clinicians
- Detailed clinical history and physical examination
- Water challenge test to confirm diagnosis
- Educate patients on the non-allergic nature and management strategies
- Referrals: dermatology, allergy/immunology, rheumatology (for autoimmune involvement)
Conclusion
AU’s rarity poses diagnostic and management challenges. Multiple pathophysiological mechanisms likely coexist, reflecting clinical variability. A structured yet flexible treatment approach, informed by emerging evidence and acknowledging patient-specific factors, provides the best path forward. Enhanced documentation and research collaboration will drive future improvements in patient outcomes and understanding of this unique condition.
Research on AU in the past 5 years consists mainly of compiled case data and novel single-case reports, given the condition’s rarity. Peer-reviewed findings from 2019–2024 have refined what we know about triggers, demographics, and treatment outcomes:
- Systematic Review (2022): Rujitharanawong et al. performed a comprehensive review of 59 papers (77 AU patients) published to dateaaaai.orgaaaai.org. They observed a strong female predominance and an average age of ~20 years at onsetpubmed.ncbi.nlm.nih.gov. Importantly, this study introduced a classification of “familial” vs. “acquired” aquagenic urticaria – about 18% of cases had a family history suggesting a genetic component, whereas ~82% were sporadicpubmed.ncbi.nlm.nih.gov. No consistent differences in triggers or symptoms were found between familial and non-familial cases. Common triggers included tap water (most frequently), as well as body fluids like sweat, saliva, and tears in some patientsaaaai.org. All patients tested positive with a standard water provocation test. On treatments, the review found that second-generation H1-antihistamines were the most reliable therapy, with many patients achieving significant improvement on daily antihistaminespubmed.ncbi.nlm.nih.gov. Topical barrier creams were reported in a few cases but with mixed results, and their efficacy remains “controversial”pubmed.ncbi.nlm.nih.gov. The authors conclude that 2nd-gen antihistamines should remain first-line for AU, and they call for further studies to address remaining knowledge gapsaaaai.org. (Source: J. Allergy Clin. Immunol. Practice, Aug 2022)
- Case Reports of Novel Therapies: Multiple recent case reports have explored advanced treatments:
- Omalizumab Case (2022): Kaur et al. reported on a teenager with refractory AU whose hives resolved with monthly omalizumab injectionspmc.ncbi.nlm.nih.gov. This case, published in BMJ Case Reports (2022), is a proof-of-concept that targeting IgE can help AU, mirroring its success in other chronic urticarias. The patient remained hive-free on omalizumab for over a year, whereas she had failed maximal antihistamine therapypmc.ncbi.nlm.nih.gov. This suggests a role for IgE-mediated processes in AU and supports omalizumab as a viable second-line treatment.
- Phototherapy Case (2021): A case series (cited in the 2022 review) noted that narrowband UVB phototherapy led to symptom improvement in two AU patients who did not fully respond to antihistaminespmc.ncbi.nlm.nih.gov. After several weeks of phototherapy, these patients tolerated water exposure with reduced whealing. While only a few cases, it indicates phototherapy may induce a partial remission by altering skin reactivity.
- Combination Therapy (2020): Some clinicians have reported success using dual antihistamine therapy (H1 + H2 blockers). For example, combining cetirizine with ranitidine (an H2 blocker) was noted to further reduce hive formation in one casepmc.ncbi.nlm.nih.gov. Though H2 antagonists alone don’t stop AU, they might provide an additive benefit to H1 blockers in select patients.
- Severe Systemic Case (2024): Ivanoff et al. published a dramatic case of a 28-year-old woman with aquagenic urticaria who experienced systemic immune complications, including episodes of anaphylaxis and a form of urticarial vasculitis concurrent with her AUresearchgate.net. Notably, this patient also had underlying lupus (SLE). The case, appearing in J. Oral & Maxillofacial Surgery, Medicine, and Pathology (2024), underscores the potential complexity of AU in the context of autoimmunity. The patient required immunosuppressive therapy to manage the vasculitic component. While exceptionally rare, this report expands the understanding of AU’s possible associations (showing it can, in isolated instances, overlap with autoimmune urticarial syndromes). It also reinforces the need for physicians to evaluate for other diagnoses (like urticarial vasculitis) if an AU patient has atypical features such as pain, prolonged lesions, or systemic signsscholar.google.com.

