The Promise and Reality of 3D-Bioprinted Cancer Models: A Technology Assessment
INGA314.AI analysis
https://www.sciencedirect.com/science/article/pii/S0169409X25001553?via%3Dihub
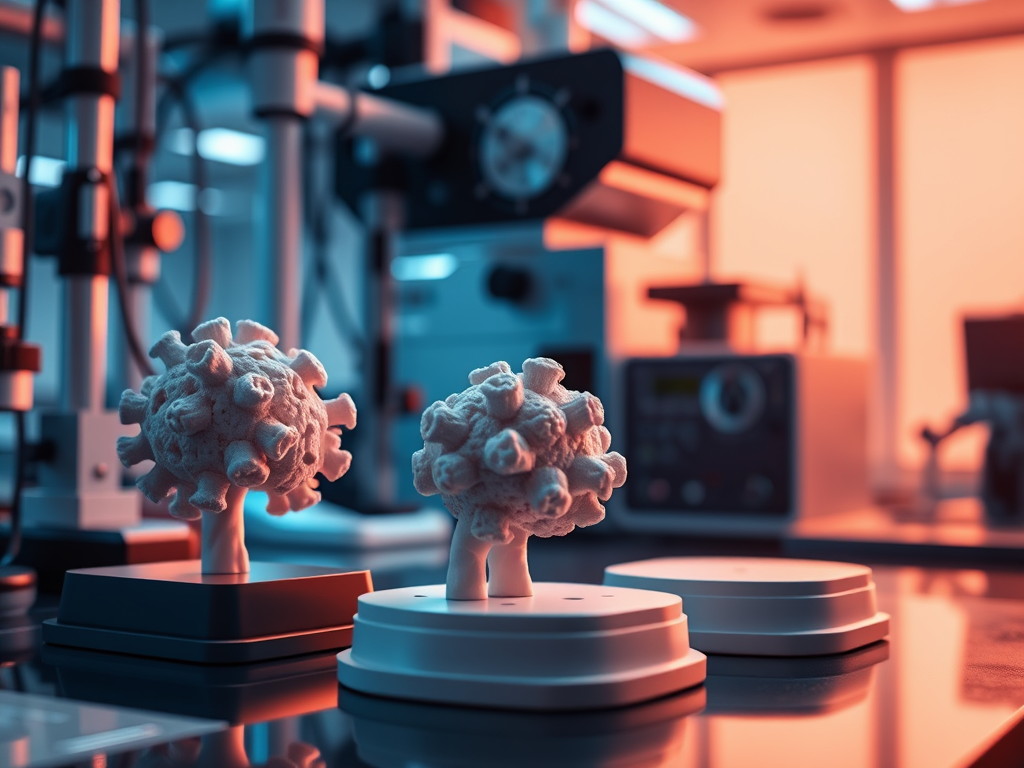
The Promise and Reality of 3D-Bioprinted Cancer Models: A Technology Assessment
Inside the cutting-edge world of printing living tumors in the lab—and what it might mean for cancer treatment
Imagine being able to print a copy of a patient’s tumor in the laboratory, complete with cancer cells, supporting tissue, and the complex architecture that makes each tumor unique. Then imagine testing dozens of different drugs on that printed tumor to see which ones work best—all before the patient receives their first treatment.
This isn’t science fiction. It’s 3D bioprinting for cancer research, and it’s happening now in laboratories around the world.
What Is 3D Bioprinting for Cancer?
3D bioprinting is essentially using specialized 3D printers to build living tissue structures layer by layer. Instead of printing with plastic or metal, these printers use “bioinks”—liquid mixtures containing living cells, proteins, and materials that mimic the natural environment where cells live.
For cancer research, scientists are using this technology to create tumor models that more closely resemble real cancers than anything we’ve had before.
How It Actually Works
The Process:
- Bioink preparation: Mix cancer cells from patients with specialized hydrogels that mimic tumor tissue
- Design: Create a 3D blueprint of the tumor structure
- Printing: Use precise robotic systems to deposit the cell-laden bioink layer by layer
- Maturation: Allow the printed construct to develop over days or weeks
- Testing: Apply different drugs and measure responses
The Result: A 3D structure containing living cancer cells arranged in patterns that mirror how tumors actually grow in patients.
The Pancreatic Cancer Challenge
Pancreatic cancer presents one of medicine’s greatest challenges, which makes it an ideal test case for advanced modeling technologies.
Why Pancreatic Cancer Is So Difficult
- Dense, fibrous tissue surrounds the cancer cells (up to 85% of the tumor)
- Poor blood supply makes it hard for drugs to reach cancer cells
- Aggressive biology with rapid spread and resistance to treatment
- Late diagnosis in most patients
- 5-year survival rate of only 8%
Why Current Models Fall Short
- 2D cell cultures: Cancer cells grow on plastic dishes, nothing like real tumors
- Mouse models: Different species, takes months to grow, expensive
- Simple 3D cultures: Better than 2D but lack the complexity of real tumors
Traditional models miss the critical interactions between cancer cells and their surrounding tissue—interactions that drive drug resistance and tumor growth.
What 3D Bioprinting Brings to the Table
Technical Capabilities
Spatial Control: Unlike other 3D models where cells organize randomly, bioprinting allows precise placement of different cell types. Cancer cells can be printed in the center with supporting fibroblasts around them, mimicking real tumor architecture.
Material Sophistication: Modern bioinks can replicate the stiffness, composition, and even some of the chemical signaling of real tumor tissue. Some are made from actual tumor tissue that’s been processed to remove cells but keep the structural framework.
Scalability: Once optimized, bioprinting can produce dozens of identical tumor models rapidly, enabling systematic drug testing that wasn’t possible before.
Patient Specificity: Models can be made using a patient’s own cancer cells and tissue, potentially enabling personalized drug testing.
Real Performance Data
Recent studies show impressive capabilities:
- 94% genetic similarity to original patient tumors maintained
- Drug response patterns that correlate with patient outcomes
- Chemoresistance profiles similar to what doctors see clinically
- Multi-week viability allowing extended drug testing
Current Limitations and Technical Challenges
The Vascularization Problem
The Challenge: Real tumors have blood vessels (albeit dysfunctional ones). Printed models largely don’t.
Why It Matters: Blood vessels affect drug delivery, oxygen levels, and how tumors grow.
Current Status: Some progress on printing channels and adding endothelial cells, but fully functional vasculature remains elusive.
Complexity vs. Simplicity Trade-offs
The Reality: Pancreatic tumors contain dozens of different cell types in complex arrangements. Current printed models use simplified versions with 2-4 cell types.
The Question: How much complexity is needed for useful predictions?
The Evidence: Even simplified models show promising correlations with patient responses, suggesting perfect complexity may not be necessary.
Material Science Gaps
The Challenge: Creating bioinks that truly mimic tissue properties while remaining printable.
Current Solutions: Hybrid approaches combining natural materials (like processed tumor tissue) with synthetic materials for printability.
Remaining Issues: No single material perfectly captures all the properties of pancreatic tumor tissue.
The “Biomimetic” Reality Check
One of the most revealing aspects of current 3D bioprinting research is how scientists describe their materials—and the logical puzzle this creates.
The Language vs. Reality Gap
What you’ll often read: Researchers describe their synthetic bioinks as “biomimetic” and “ECM-mimetic”—terms suggesting they successfully mimic biological tissue.
What the same papers then reveal: Natural materials derived from actual tumor tissue “closely mimic the native tumor microenvironment” better than synthetic alternatives.
The final admission: “No single formulation meets all the necessary conditions.”
What This Actually Tells Us
This isn’t scientific doublespeak—it’s the honest complexity of developing new technology:
Synthetic bioinks are “biomimetic” compared to previous synthetic materials, but still fall short of biological reality.
Natural tumor-derived materials are closer to the real thing but come with their own limitations—batch variability, processing challenges, and limited availability.
The current state: We’re making significant progress toward truly biomimetic materials, but we’re not there yet.
Why Precision in Language Matters
This distinction is more than academic. It affects:
- Research priorities: Are we perfecting current synthetic approaches or developing fundamentally new materials?
- Clinical expectations: How close are we really to tumor models that accurately predict patient responses?
- Investment decisions: Where should funding and resources be directed?
The honest assessment: Current bioprinted models are major improvements over previous approaches and show promising clinical correlations, but they’re still approximations of tumor biology rather than true replications.
What the Technology Can Do Today
Research Applications
- Drug screening: Test multiple compounds on tumor models
- Combination therapy optimization: Find the best drug combinations
- Resistance mechanism studies: Understand why treatments fail
- New target identification: Discover new therapeutic approaches
Emerging Clinical Potential
- Treatment selection: Help choose the best available therapy for individual patients
- Drug development: Better preclinical testing could improve clinical trial success rates
- Personalized medicine: Eventually enable truly individualized treatment approaches
The Timeline Reality
What’s Happening Now (2025)
- Research tool refinement: Improving bioinks, printing techniques, and model complexity
- Validation studies: Testing how well model predictions correlate with patient outcomes
- Scaling efforts: Making the technology more accessible and standardized
Near-term prospects (2-5 years)
- Clinical validation trials: Large studies testing whether model-guided treatment improves patient outcomes
- Technology optimization: Better materials, faster printing, more reliable predictions
- Regulatory pathway development: FDA and other agencies developing frameworks for approval
Longer-term potential (5-10 years)
- Clinical implementation: Routine use in cancer centers for treatment selection
- Expanded applications: Use in other cancer types and diseases
- Integration with other technologies: Combination with AI, genomics, and other precision medicine tools
Economic and Practical Considerations
Current Costs
- Equipment: Specialized bioprinters cost $50,000-$500,000
- Materials: Bioinks and culture media add ongoing costs
- Expertise: Requires trained technicians and specialized facilities
- Time: 2-4 weeks from tissue sample to results
Scalability Questions
- Patient access: Currently limited to research centers
- Tissue requirements: Need adequate tumor samples (challenging in pancreatic cancer)
- Throughput: How many patients can be served?
- Cost-effectiveness: Will insurance cover model-based treatment selection?
The Competitive Landscape
3D bioprinting isn’t the only approach to better cancer modeling:
Alternative Technologies
- Organoids: Self-organizing 3D cultures (faster, cheaper, but less control)
- Organ-on-chip: Microfluidic devices with flow and multiple tissues
- Advanced imaging: Better analysis of existing tumors
- Computational modeling: AI-based prediction without physical models
Complementary Approaches
Rather than competing, these technologies may work together:
- Bioprinting + Organoids: Use printing to organize organoid components
- Models + AI: Combine physical and computational modeling
- Multiple platforms: Different approaches for different questions
Technical Specifications and Capabilities
Current Bioprinting Parameters
- Resolution: 100-200 micrometers (about the width of a human hair)
- Printing speed: Minutes to hours depending on construct size
- Cell viability: 85-95% of cells survive the printing process
- Model size: From millimeter spheroids to centimeter-scale constructs
Material Properties
- Stiffness range: Can mimic tissue stiffness from soft (brain-like) to firm (cartilage-like)
- Composition: Combinations of collagen, hyaluronic acid, gelatin, and other biological materials
- Degradation: Materials can be designed to break down over time like real tissue
Future Directions
Technical Improvements
- 4D bioprinting: Materials that change properties over time
- Multi-material printing: Simultaneously printing different tissue types
- Improved vasculature: Better methods for creating functional blood vessels
- Real-time monitoring: Sensors embedded in printed tissues
Material Science Evolution
The “biomimetic gap” is driving innovation in several directions:
- Hybrid materials: Combining the best of synthetic and natural approaches
- Smart materials: Bioinks that respond to biological signals
- Personalized matrices: Materials derived from individual patient tissues
- Dynamic systems: Models that change and remodel like real tissues
Application Expansion
- Other cancer types: Adapting approaches for breast, lung, brain cancers
- Drug development: Use in pharmaceutical research
- Immunotherapy testing: Models that include immune system components
- Metastasis modeling: Understanding how cancer spreads
The Bottom Line on 3D Bioprinted Cancer Models
What this technology represents: A significant step forward in cancer research methodology that could eventually improve patient care.
What it can do now: Create more realistic tumor models for research and potentially guide treatment selection in select cases.
What it cannot do yet: Perfectly replicate tumor biology or serve as a routine clinical tool.
The material reality: Current bioinks are improvements over previous approaches but still approximations of real tissue—and researchers are honest about this when you read carefully.
The realistic timeline: Research tool today, potential clinical application in 5-10 years with proper validation and continued material development.
The potential impact: If successful, could transform how we select cancer treatments, leading to better outcomes and fewer futile therapies.
For Patients and Families
If you or a loved one is facing pancreatic cancer, here’s what this technology means:
Today: This is promising research that may eventually improve treatment options, but it’s not yet clinically available.
Tomorrow: Clinical trials may become available to test whether model-guided treatment improves outcomes.
The future: This could become a standard part of cancer care, helping doctors choose the best treatments for each individual patient.
The takeaway: Real progress is being made in cancer research. Current models aren’t perfect replications of tumors, but they’re showing promising correlations with patient responses—and that’s progress worth building on.
3D bioprinting for cancer represents one of many promising approaches being developed to tackle humanity’s most challenging diseases. The technology is advancing rapidly, but honest assessment of current capabilities—including the gap between synthetic “biomimetic” materials and biological reality—is crucial for setting appropriate expectations and directing research priorities. For the first time, we can literally print approximations of tumors and test treatments before patients receive them. That’s remarkable progress, even if it’s not yet perfect replication.

